A global health crisis
Lead the way in the fight against resistance
From the moment they were discovered, antibiotics have transformed medicine, and saved millions of lives1
However, the rapid emergence of antibiotic resistance is threatening the very existence of these life-saving drugs, and their benefit to you, and your patients.1 Meaning, considering the right drug, dose and duration is now more essential than ever in tackling this health crisis2,3
With dermatology being the top antibiotic prescriber specialty in the U.S., you are uniquely positioned to take the lead in what has become a global fight against antibiotic resistance5–7
By continuing to uphold your responsibility to antibiotic stewardship, you can help protect the future of these vital medicines for generations to come2,8
10 million lives
Antibiotic resistance is on track to claiming 10 million lives a year by 2050. That is 10 million people dying from previously-treatable bacterial infections4
Your choices today, could transform
their tomorrows
Antibiotic resistance has now become a universal threat. It can affect anyone, of any age, in any country, making us all key in the fight against it6,9
Act now against antibiotic resistance10
![]()
Right drug
![]()
Right dose
![]()
Right duration


Without action
Without effective antibiotics, currently safe procedures like organ transplantations, chemotherapy, and
surgeries become life-threatening, and other infectious diseases may become difficult to treat. Without a
real change in prescribing behavior, we are putting the achievements of
modern medicine, and the lives of many, at risk2,5

In the U.S. alone, each year at least 2.8 million people get an antibiotic-resistant infection2

Economic losses of about $35 billion annually have been recorded, related to lost productivity, due to antibiotic resistances in U.S. healthcare systems alone11

Methicillin-resistant Staphylococcus aureus (MRSA) infections alone, among the highest of all antibiotic-resistance threats, are said to cost the U.S. healthcare system ~$60,000 per patient and ~$9.7 billion a year12
ANTIBIOTIC MISUSE
The problem we are facing is real
Without a real change in prescribing behavior, we risk the effectiveness of our antibiotics2,5
What are currently safe medical procedures, could become life-threatening2,5
Did you know, in the U.S.:

oral antibiotic prescriptions are prescribed for dermatological conditions every year, with dermatologists prescribing antibiotics more commonly than any other physician group6

of all oral antibiotics prescribed by dermatologists are tetracyclines, particularly doxycycline and minocycline6

of patients prescribed antimicrobials in dermatology are individuals with acne or rosacea5
Without urgent action, antibiotic resistance could claim
10 million lives a year by 20504
The science behind antibiotic resistance
How do bacteria develop antibiotic resistance?13
![]()
There are lots of bacteria, and a few are resistant to antibiotics
![]()
When antibiotics kill bacteria causing illness, they also kill good bacteria protecting the body from infection
![]()
The antibiotic-resistant bacteria grow and take over
![]()
Some bacteria give their antibiotic resistance to other bacteria, causing more problems
Antibiotics fight bacteria, however they can fight back and find
new ways to survive. These defense strategies are called
resistance mechanisms. Only the bacteria, not people, become
resistant to antibiotics2
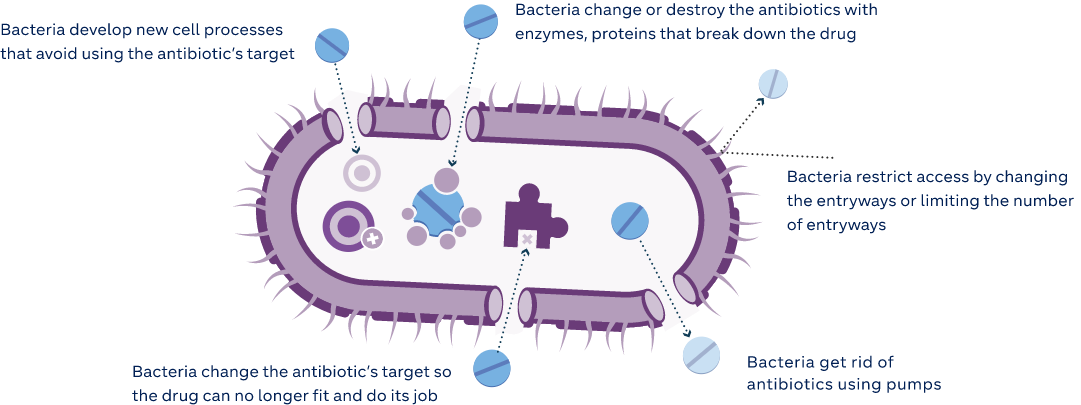
Visuals adapted from: Centers for Disease Control and Prevention (CDC)2,13
How can antibiotic resistance emerge and spread in a healthcare setting?
A typical path for the emergence of antibiotic-resistant bacteria, and the subsequent spread throughout
a healthcare facility could look like:14
1
Patient receives antibiotics
2
The bacteria in the gut are killed, unless they have a gene for resistance
3
With little competition, those bacteria now flourish
4
The patient visits a hospital, and uses the bathroom, failing to wash their hands properly
5
Someone else touches something this patient has been in contact with, and contracts the resistant infection
The resistant bacteria can then spread from patient to patient, or on medical equipment, and into sterile, surgical environments14
Adapted from: Antibiotic Research UK14
Signs and symptoms of resistance
The consequences of resistance related to antibiotic-use may not always be readily detectable or easy
to spot by you or your patients.6 However, in dermatology, where high doses of antibiotics can be used
for a long period of time, signs of resistance may include:5,15,16
- Treatment failure of skin conditions in response to antibiotics
- Disturbance in the normal flora of the skin,* and other places in the
body, possibly increasing chances of infections, such as upper
respiratory tract infection - The introduction and growth of opportunistic pathogens, locally and
systemically
Generally, antibiotic-resistant skin infections may present in patients
the same as any other common infection – the infected area is usually:17
![]()
Red
![]()
Hot
![]()
Painful
![]()
In some cases, a patient might have a fever, or feel hot and cold
Antibiotic-resistant infections will not respond to the antibiotics most often used to treat it, though there
may be others that can be used. With these infections, a swab test can help identify which bacteria are
present, and the best antibiotic(s) to use17
*Culture and susceptibility testing before and after antibiotic treatment can help identify changes in skin flora and the
presence, type and severity of resistance bacteria, if infection is suspected15
Need for change
Everyone who depends on antibiotics must join forces to help detect and prevent the emergence, and spread of antibiotic resistance
The world urgently needs to change the way it prescribes and uses antibiotics – without behavior change, antibiotic resistance will not only remain a major threat, but an active reality2,4,9
Combating antibiotic resistance is not just a national, but a global priority, with the U.S. government, Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) all actively launching initiatives, supporting research and outlining guidance, with hopes to tackle the devastating threat that antibiotic resistance poses2,18,19
“Fighting this threat is a public health priority. It requires a collaborative global approach across sectors to detect, prevent, and respond to these threats when they occur”
Centers for Disease Control and Prevention (CDC), 202018
As part of the ongoing battle against resistance in the U.S., the CDC proposed core actions to better prepare the nation for this threat that continues to emerge worldwide – antibiotic stewardship is an integral cornerstone in this strategy:2,8



You can confidently take the lead as an antibiotic steward in your field, by simply ensuring that the right drug, dose and duration is prescribed to your patients10,20


Act now against antibiotic resistance
Real change starts with you. Choose the right drug, dose and duration
With first-hand experience of the life-changing impact antibiotics can have on patients, and with dermatology being the top antibiotic prescriber specialty in the U.S., you are key in leading the global fight against antibiotic resistance6
Antibiotic stewardship can be used across all healthcare settings, and is the cornerstone of efforts in improving antibiotic use, and slowing the spread of resistance. The goal is to maximize the benefit of antibiotic treatment while minimizing harm both to individuals, and to communities10
What is antibiotic stewardship?
Antibiotic stewardship is the effort to measure and improve how antibiotics are prescribed by:10
- Ensuring the right drug, dose and duration are selected when an antibiotic is needed
- Prescribing and using antibiotics only when needed
- Minimizing misdiagnoses or delayed diagnoses leading to underuse of antibiotics
Centers for Disease Control and Prevention (CDC), 202010
One change in how you prescribe, is one step further in the fight against resistance:6,15
- Identify and assess whether an antibiotic is truly needed
- Consider sub/non-antibiotic alternatives where possible
- Consider the shortest regimen required to treat
Continue to ask your patients if they have been on an antibiotic (what dose and duration) in the past 12 months to avoid cumulative effects of any medication
Take action against antibiotic resistance
Aside from opting for the right drug, dose and duration, there are
more ways you can uphold your commitment to antibiotic stewardship,
and help decelerate the threat in this fight against antibiotic
resistance10,21
Prevent and control
- Help prevent infections, and their spread by continuing to follow infection prevention and control guidelines (ensuring hands, instruments, and environment are clean)21
- Stay informed of current infection outbreaks, and aware of resistance patterns using available surveillance tools21,22
Educate
- Talk to your patients about how to take antibiotics correctly, antibiotic resistance, and the dangers of misuse10,21
- Provide patient education materials:10
- On appropriate antibiotic use
- On potential adverse drug events from antibiotics5
- On the management of common infections
Self-evaluate
- You can use self-evaluations to align antibiotic prescribing practices with updated evidence-based recommendations and clinical practice guidelines10
- If you were to come across antibiotic-resistant infections, your valuable report to surveillance teams could guide changes in practice, and be used to assess progress in improving antibiotic prescribing22
- Be aware of infections, and resistance patterns in your direct facility, and community21
- Ensure you are notified immediately when antibiotic-resistant germs are identified in your patients21



By considering sub-antibiotic dose treatments, you are not only offering your patients effective options, but also choosing to protect future health by opting for a treatment that does not contribute to antibiotic resistance20,23


STAY CONNECTED
Sign up and
stay up-to-date
For the latest news, research, and insights into papulopustular rosacea, subscribe now! You’ll also receive patient resources and toolkits, helping you treat your patients throughout their rosacea journey
Important Safety Information
Indication: ORACEA® (doxycycline) 40 mg* capsules are indicated for the treatment of only inflammatory lesions (papules and pustules) of rosacea in adult patients. ORACEA does not lessen the facial redness caused by rosacea. Adverse Events: In controlled clinical studies, the most commonly reported adverse events (>2%) in subjects treated with ORACEA were nasopharyngitis, diarrhea, hypertension and sinusitis. Warnings/Precautions: ORACEA should not be used to treat or prevent infections. ORACEA should not be taken by patients who have a known hypersensitivity to doxycycline or other tetracyclines. ORACEA should not be taken during pregnancy, by nursing mothers, or during tooth development (up to the age of 8 years) and may cause reversible inhibition of bone growth. If Clostridium difficile associated diarrhea (CDAD) occurs, may need to discontinue ORACEA. Although photosensitivity was not observed in clinical trials, ORACEA patients should minimize or avoid exposure to natural or artificial sunlight. The efficacy of ORACEA treatment beyond 16 weeks and safety beyond 9 months have not been established.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
*30 mg immediate release and 10 mg delayed release beads
REFERENCES
1. Ventola CL. The antibiotic crisis. Part 1: Causes and threats. P&T 2015;40:277–283. 2. Centers for Disease Control and Prevention 2020. Antibiotic resistances threats in the United States 2019. Available at: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf. Last accessed: September 2021 3. Paterson IK, et al. Optimising antibiotic usage to treat bacterial infections. Scientific Reports 2016;6:37853. DOI: https://doi.org/10.1038/srep37853. 4. World Health Organization 2019. No time to wait: Securing the future from drug-resistant infections. Available at: https://www.who.int/publications/i/item/no-time-to-wait-securing-the-future-from-drug-resistant-infections. Last accessed: September 2021. 5. Karadag AS, et al. Antibiotic resistance in acne: Changes, consequences and concerns. JEADV. 2020. https://doi.org/10.1111/jdv.16686. 6. Del Rosso JQ, et al. Status report from the Scientific Panel on Antibiotic Use in Dermatology of the American Acne and Rosacea Society: Part 1. J Clin Aesthet Dermatol. 2016;9(4):18–24. 7. Barbieri JS, et al. Trends in oral antibiotic prescription in dermatology, 2008 to 2016. JAMA Dermatol. 2019;155:290–297. 8. Centers for Disease Control and Prevention 2020. Antibiotic resistance questions and answers. Available at: https://www.cdc.gov/antibiotic-use/community/about/antibiotic-resistance-faqs.html. Accessed: September 2021. 9. World Health Organization 2020. Antibiotic resistance. Available at: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance. Last accessed: September 2021. 10. Centers for Disease Control and Prevention 2019. The core elements of outpatient antibiotic stewardship. Available at: https://www.cdc.gov/antibiotic-use/community/pdfs/16_268900-A_CoreElementsOutpatient_508.pdf. Last accessed: September 2021. 11. Aslam B, et al. Antibiotic resistance: A rundown of a global crisis. Infection and Drug Resistance 2018;11:1645–1658. 12. Infection Control Today 2015. MRSA: The superbug poised to cost hospitals super sums. Available at: https://www.infectioncontroltoday.com/view/mrsa-superbug-poised-cost-hospitals-super-sums. Last accessed: September 2021. 13. Centers for Disease Control and Prevention 2020. How antibiotic resistances happens. Available at: https://www.cdc.gov/antibiotic-use/week/pdfs/How_Antibiotic_Resistance_Happens_508.pdf. Accessed: September 2021. 14. Antibiotic Research UK. Antibiotic-resistant bacteria in healthcare. Available at: https://www.antibioticresearch.org.uk/about-antibiotic-resistance/antibiotic-resistant-bacteria-in-healthcare/. Last accessed: September 2021. 15. Del Rosso JQ, et al. Status report from the Scientific Panel on Antibiotic Use in Dermatology of the American Acne and Rosacea Society: Part 3. J Clin Aesthet Dermatol. 2016;9(6):17–24. 16. Garrett JPD and Margolis DJ. Impact of long-term antibiotic use for acne on bacterial ecology and health outcomes: A review of observational studies. Curr Derm Rep. 2012;1:23–28. 17. Antibiotic Research UK. About antibiotic-resistant skin and soft tissue infections. Available at: https://www.antibioticresearch.org.uk/find-support/skin-soft-tissue-infections/. Last accessed: September 2021. 18. Centers for Disease Control and Prevention 2020. Combat antimicrobial resistance globally. Available at: https://www.cdc.gov/drugresistance/intl-actvities.html. Accessed: September 2021. 19. Centers for Disease Control and Prevention 2019. U.S action to combat antibiotic resistance: A national priority. Available: https://www.antibioticresearch.org.uk/find-support/skin-soft-tissue-infections/. Last accessed: September 2021. 20. Schaller M, et al. State of the art: Systemic rosacea management. J Dtsch Dermatol Ges. 2016;14:29–37. 21. Centers for Disease Control and Prevention 2020. Protecting patients and stopping outbreaks. Available at: https://www.cdc.gov/drugresistance/us-activities.html. Last accessed: September 2021. 22. World Health Organization. Global Antimicrobial Resistance Surveillance System (GLASS). Available at: https://www.who.int/publications/i/item/global-antimicrobial-resistance-surveillance-system-(-glass)-report. Last accessed: September 2021. 23. Del Rosso JQ, et al. Status report from the Scientific Panel on Antibiotic Use in Dermatology of the American Acne and Rosacea Society: Part 2. J Clin Aesthet Dermatol. 2016;9(5):11–17